
Keratoconus
What is Keratoconus ?
A clinical condition characterised by thinning and forward protrusion of the cornea resulting in
conical shape. This disorder is usually bilateral, with onset at the age of 10 -14 years. Affects both
sexes, with a slight female preponderance. Although it has been reported in families, the risk of
inheritance is reasonably low.
Why does is occur ?
Etiology of this condition is still not clear. It is possible that this condition could be secondary to
increased breakdown of the stromal collagen lamellae by the lysosomal enzymes released by the
basal epithelium in these eyes.
What is Keratoconus ?
A clinical condition characterised by thinning and forward protrusion of the cornea resulting in
conical shape. This disorder is usually bilateral, with onset at the age of 10 -14 years. Affects both
sexes, with a slight female preponderance. Although it has been reported in families, the risk of
inheritance is reasonably low.
Why does is occur ?
Etiology of this condition is still not clear. It is possible that this condition could be secondary to
increased breakdown of the stromal collagen lamellae by the lysosomal enzymes released by the
basal epithelium in these eyes.

| Keratoconus is characterized by central thinning and forward protrusion of the cornea. |




| Keratoconus patients with good unaided vision following DALK surgery. None of them are using contact lenses anymore |
| Angulation of the lower lid in downgaze known as Munson's sign, which is a nonspecific sign of advanced keratoconus |
Fig - Keratoconus. The thinning is most pronounced at the apex of the cone, which is
usually inferior to the visual axis. The cornea is thinnest at the region of maximal protrusion
usually inferior to the visual axis. The cornea is thinnest at the region of maximal protrusion


| Milind (Kolkata) DALK left eye unaided vision 6/9 (20/30) |
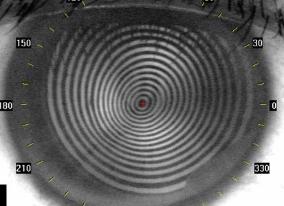
Corneal topography map showing steep area of the
cornea inferotemporally, suggestive of keratoconus
cornea inferotemporally, suggestive of keratoconus
| Photokeratoscope image showing crowding of the mires inferiorly ,(egg shaped mires) indicating steeper corneal curvature in that region |

Management
Glasses can be prescribed to correct the induced astigmatism in early keratoconus. Once
the cylindrical power increases beyond 4.0 diopters, patients find it difficult to tolerate such
high power in glasses.
Semisoft or RGP or Rose K contact lens, can help in cases with mild to moderate
keratoconus. The front surface of the contact lens now acts like the front surface of the
cornea with a regular shape. This provides reasonably clear vision for normal daily
activities. However, fitting of contact lens in eyes with keratoconus requires expertise in CL
fitting and a special set of trial lenses. With increasing progression of keratoconus, patients
may find it difficult to wear the contact lens, and at times the lens keeps falling out of the
eye. In such situations, piggy back lens ie RGP lens mounted on a soft contact lens can be
tried.
Glasses can be prescribed to correct the induced astigmatism in early keratoconus. Once
the cylindrical power increases beyond 4.0 diopters, patients find it difficult to tolerate such
high power in glasses.
Semisoft or RGP or Rose K contact lens, can help in cases with mild to moderate
keratoconus. The front surface of the contact lens now acts like the front surface of the
cornea with a regular shape. This provides reasonably clear vision for normal daily
activities. However, fitting of contact lens in eyes with keratoconus requires expertise in CL
fitting and a special set of trial lenses. With increasing progression of keratoconus, patients
may find it difficult to wear the contact lens, and at times the lens keeps falling out of the
eye. In such situations, piggy back lens ie RGP lens mounted on a soft contact lens can be
tried.

| Janani (Chennai) DALK both eyes unaided vision 6/9 (20/30) |
| Semisoft or RGP contact lens wear in an eye with moderate Keratoconus. |

| Collagen crosslinking or C3R or CXL This is a new modality of treatment for keratoconus, where in Riboflavin eye drops are applied followed by exposure of the cornea to ultraviolet radiation for a duration of 30 minutes. This results in cross linking of the collagen fibres of the cornea, thereby increasing its physical strength by upto 300%. Thus further progression of keratoconus can be arrested, and in 15 -20% cases regression has also been noted. Longest followup duration following this treatment is for 10 years. A variety of options for collagen crosslinking treatment are now available at Cornea Clinic, Apollo Hospitals, Hyderabad. |
| Ahmed (Kerala) DALK left eye unaided vision 6/9 (20/30) |
| Intacs implants This is a newer surgical treatment for mild to moderate keratoconus. In this surgery, fine plastic implants are placed in the peripheral cornea, which helps flatten the central cornea, thereby improving the unaided vision. Patients are able to return back to normal glass wear or comfortable contact lens wear post treatment. This procedure is painless and simple to perform. The surgery is performed under topical anesthesia using the Ziemer Z6 femtosecond laser, and takes only 5 -10 minutes per eye. |

Surgical treatment
Surgical intervention is often necessary in advanced Keratoconus to restore corneal anatomy and thereby improve quality of
vision.
Traditionally full thickness corneal transplantation procedures have been commonly performed for advanced keratoconus.
Although this procedure has successful outcome in a large number of cases, it sacrifices the healthy endothelium of the host
cornea. The transplanted donor cornea is at risk for rejection,and requires steroid therapy for a long duration to prevent
rejection. This predisposes the eye to steroid induced complications such as cataract and glaucoma.
Surgical intervention is often necessary in advanced Keratoconus to restore corneal anatomy and thereby improve quality of
vision.
Traditionally full thickness corneal transplantation procedures have been commonly performed for advanced keratoconus.
Although this procedure has successful outcome in a large number of cases, it sacrifices the healthy endothelium of the host
cornea. The transplanted donor cornea is at risk for rejection,and requires steroid therapy for a long duration to prevent
rejection. This predisposes the eye to steroid induced complications such as cataract and glaucoma.
| Ms Joshi (Jamshedpur) DALK right eye unaided vision 6/9 (20/30) |

Deep Anterior Lamellar Keratoplasty (DALK)
With advancement in corneal surgical techniques, it is now possible to selectively
remove the anterior layers from the cornea and replace it with donor tissue to
restore its anatomy and function. Deep anterior lamellar keratoplasty (DALK) is
one such procedure wherein the host corneal endothelium is retained, and anterior
corneal tissue is replaced with normal thickness donor tissue. As the host
endothelium is retained there is no risk of rejection, and steroids have to be
given only for a short duration of time. However DALK surgery requires more
surgical expertise compared to the traditional full thickness keratoplasty, and hence
performed by only well trained corneal surgeons all over the world.
With advancement in corneal surgical techniques, it is now possible to selectively
remove the anterior layers from the cornea and replace it with donor tissue to
restore its anatomy and function. Deep anterior lamellar keratoplasty (DALK) is
one such procedure wherein the host corneal endothelium is retained, and anterior
corneal tissue is replaced with normal thickness donor tissue. As the host
endothelium is retained there is no risk of rejection, and steroids have to be
given only for a short duration of time. However DALK surgery requires more
surgical expertise compared to the traditional full thickness keratoplasty, and hence
performed by only well trained corneal surgeons all over the world.
| Archana (Mumbai) DALK left eye unaided vision 6/9 (20/30) |


In advanced stages of Keratoconus, due to extreme thinning, the inner layer of the
cornea can rupture, leading to increased leakage of fluid into the cornea. This
results in whitening of the cornea, with sudden decrease in vision. This condition is
called acute hydrops. In this situation, topical medications have to be applied for
symptomatic relief. It takes 3 - 4 months for the corneal oedema to resolve, following
which a standard full thickness keratoplasty is required to restore corneal clarity and
visual improvement. Specialised penetrating keratoplasty using Ziemer Z6
femtosecond laser allows customized grafts to be prepared and transplanted.
It this situation lamellar surgery is not recommended, and hence one should not wait
for this complication to occur, and take advantage of lamellar procedures at an
early stage.
cornea can rupture, leading to increased leakage of fluid into the cornea. This
results in whitening of the cornea, with sudden decrease in vision. This condition is
called acute hydrops. In this situation, topical medications have to be applied for
symptomatic relief. It takes 3 - 4 months for the corneal oedema to resolve, following
which a standard full thickness keratoplasty is required to restore corneal clarity and
visual improvement. Specialised penetrating keratoplasty using Ziemer Z6
femtosecond laser allows customized grafts to be prepared and transplanted.
It this situation lamellar surgery is not recommended, and hence one should not wait
for this complication to occur, and take advantage of lamellar procedures at an
early stage.
| Khalid (Oman) DALK right eye unaided vision 6/12 (20/40) |

| Acute hydrops in Keratoconus - Note the corneal opacification and oedema at the apex of cornea |

| Standard full thickness corneal transplantation procedure, is very successful in restoring corneal structure and function. However one needs to use topical steroids for a longer duration than lamellar procedures. Full thickness corneal grafts in keratoconus have the best clinical outcome, when compared with other indication of corneal transplantation surgery. |
| Najeeba (Kerala) DALK both eyes unaided vision 6/9, 6/12 (20/30, 20/40) |
| Standard full thickness keratoplasty for Keratoconus |
Dr Rajesh Fogla, senior corneal surgeon has special interest in keratoconus disorder and its management. He has a vast experience in contact lens fitting, & specialized corneal procedures to effectively manage this condition. He has been performing Deep Anterior Lamellar Keratoplasty since 1998, & has numerous publications & presentations on the same For more information regarding the cost of surgery and other details you can email Dr Rajesh Fogla at dr_fogla@yahoo.com or call him on +91 9866076750 |

| Clinical features Clinical presentation is usually with progressive visual symptoms secondary to corneal changes. Irregular astigmatism results in blurred vision, glare, and diplopia. Glasses do not help improve vision, and rigid contact lens wear is required for improving eyesight. |
| Tel 91 40 23607777, Fax 91 40 23608050 ,24 hours emergency services call 1066 |
| Cornea Clinic - Eye Department - Apollo Hospitals, Jubilee Hills, Hyderabad 500096, Telangana, INDIA |
| Cornea Clinic - toll free number 1600 345 1066, other numbers 91 40 23607777 ext 6333 |
| www.corneaclinic.com |
| www.corneaclinic.com |
| www.corneaclinic.com |
| www.corneaclinic.com |
| www.corneaclinic.com |
| www.corneaclinic.com |
| www.corneaclinic.com |
| www.corneaclinic.com |
| www.corneaclinic.com |
| www.corneaclinic.com |
| Phakic IOL implantation surgery This is a new modality of treatment in keratoconus patients to improve unaided vision. Phakic IOL such as Staar Toric ICL helps reduce the refractive error and astigmatism thereby significantly improving unaided vision. Patients are able to do away with contact lens wear or dependence on glasses. However not all keratoconus patients are suitable for this modality of treatment. You can email your reports to Dr Fogla to know if you are eligible for the phakic IOL. |

| Cornea Clinic |

| Center for Innovative Corneal Surgery |



